Every time when I hear the term fibromyalgia, I always need to look up what it means, its pathophysiology, clinical presentations and its guidelines and management strategies. In fact, Hauser et al recently published a review article, looking at the management of fibromyalgia. The authors describes the various diagnostic criteria and recommendations from Canada, Germany and Israel and highlighted how they differ to a great extent in their overall approach in symptoms description, recommended investigations and screening procedures.
Further in US alone, the diagnostic criteria have been revised at least 4 times since 1990. In the latest 2016, fibromyalgia may be diagnosed in adults when all of the following criteria are met:
- Generalized pain, defined as pain in at least 4 of 5 regions, is present.
- Symptoms have been present at a similar level for at least 3 months.
- Widespread pain index (WPI) ≥ 7 and symptom severity scale (SSS) score ≥ 5 or WPI of 4-6 and SSS score ≥ 9.
- A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses.
I can only summarize in one word, confusing! I may also add that I think the medical community really does not have a good idea what we are dealing with here, given the inconsistent approaches as well as ongoing debates on diagnosis and treatment of fibromyalgia.
However, all guidelines focus on providing patient education. Specifically, the German Guidelines suggest including the following messages in patient education:
- Reassurance that the symptoms are not caused by an organic disease (such as abnormality of the muscles or joints) but are instead based on a functional disorder of the brain(altered processing of pain and other external stimuli)
- The legitimacy of the ailment should be acknowledged. The symptoms are real.
- The symptoms are persistent in most adult patients.
- Total relief of symptoms is seldom achieved.
- The symptoms should not lead to disablement and do not shorten life expectancy.
- Most patients learn to adapt to the symptoms over time.
- The patient can learn to improve symptoms and health-related quality of life via self-management strategies.
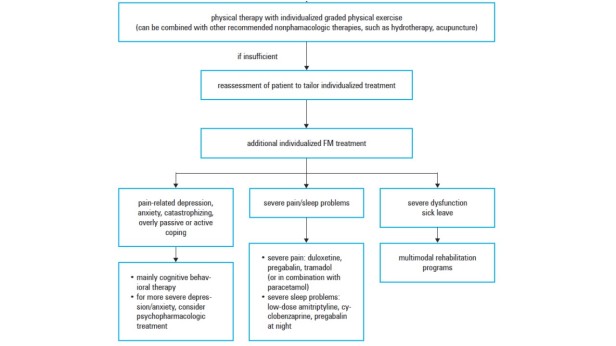
Hauser et al have also included an algorithm describing the stepwise and individualized treatment according to the European League Against Rheumatism.
The following non-pharmacological recommendations for fibromyalgia are based on the European League against Rheumatism.:
- Aerobic and strengthening training (Level 1a, strong)
- Cognitive behaviour therapies (Level 1a, weak)
- Multicomponent therapies (Level 1a, weak)
- Defined physical therapies: acupuncture or spa therapy (Level 1a, weak)
- Meditative movement therapies (qigong, yoga, tai chi) and mindfulness-based stress reduction (Level 1a, weak)
In terms of pharmacological management, the usual pain treatment options such as NSAID, acetaminophen and opioids have NOT been shown to be effective. Instead, the recommended treatments typically include pain modulators such as:
- Serotonin and noradrenaline reuptake inhibitors (e.g. duloxetine),
- Tricyclic antidepressant (e.g. amitriptyline),
- Antiepileptic agents (e.g. pregabalin).
While they are considered the recommended treatment options, they are known to be NOT very effective, with the expected pain relief to be around 10-25% in reduction.
Lawson K has recently published an article reviewing some potential drug therapies for treatment of fibromyalgia. In addition to the aforementioned options, she has also included the following:
- Antipsychotic (e.g. quetiapine)
- Glutamate (e.g. memantine)
- Substance P (e.g. capsaicin)
- Naltrexone – an opioid receptor antagonist used often in the treatment of alcohol or opioid dependence.
- Cannabinoids
- Potassium channel (e.g. flupertine – a centrally acting, non-opiate analgesic)
- Melatonin (endogenous hormone that helps with insomnia)
- IMC-1 (a fixed dose combination of famciclovir and celecoxib)
I think when we cannot decide clearly on what fibromyalgia is, it also reflects in our treatment options – we cannot find anything that works very well, so we are including so many not-so-useful options to consider.
So my bottom line is that we do not have a clear idea the cause of fibromyalgia, we cannot agree on a reliable diagnostic criteria and our treatment options include a list of drugs that we know do not work very well. There is still a lot of work to be done in understanding fibromyalgia and hopefully to find some effective treatments. In the meantime, we do not have much to offer our patients.
But perhaps the cure or the answer must come from the individual.
Recently, I have been so inspired by one blogger, Fibronocci. In her blog, she describes how having a diagnosis of fibromyalgia has changed her life. She has gone from a high functioning individual to someone who has to struggle daily with physical weakness, pain and misunderstanding by those who do not know about fibromyalgia. But her inner strength is so remarkable. I follow her blog to see how she journeys through her struggles, sets new expectations for herself as well as how she becomes more appreciative of the simple things in life. She may be physically weak but her mental strength is worthy of my admiration. Check out her blog here and her beautiful artwork!
From reading her blog, I have a deeper understanding of how some patients with chronic diseases may experience every day, beyond what I often see in their medical charts and medication profiles. In many ways, she reminds me to be humble because we – the healthcare professionals – sometimes really do not have all the answers. We should encourage patients to explore how they should claim their lives back with the coexistence of their chronic conditions. I know – it is easier said then done but a simple pill can’t fix everything. In this case, there is definitely no magic pill to cure fibromyalgia, at least not yet.

Hi Cynthia! Thank you so much for the very well-thought out article on Fibromyalgia! It’s a great education tool for many who are seeking answers in a nutshell. Thank you, also, for your kind words about me and my blog. I feel truly humbled. ❤
You may be interested in researching Dr. Dan Clauw. He's a leading FM researcher based off of Michigan. He has a great video explaining the current state of our FM understanding: https://www.youtube.com/watch?v=pgCfkA9RLrM
LikeLiked by 1 person
Thank you. I will check out the video. I feel a little risky writing it because people don’t want to admit that we don’t know what we are doing…. at least not yet. I hope you are doing well and I truly mean it when I admire your strength.
LikeLiked by 1 person
I appreciate that Cynthia – I equally admire you for pushing through your own struggles and helping others with your blog. 🙂 I fully understand why you feel risky admitting how little we know. When I tried to explain to laymen that it is a CNS condition of altered/erroneous pain processing, the first response is, “so it is ‘mental’?” I usually come back with the term “neurological” because of all the baggage associated with that phrase. But sometimes I feel like they are not trying to be belittling or dismissive, it is just hard for people with little biological knowledge to understand how you can feel pain without a pain-inducing stimulus; so they come to the conclusion that you must be imagining it or it’s “all in your head.” That’s one reason why I liked Dr. Clauw’s tongue-in-cheek talk title! 😀
LikeLiked by 1 person